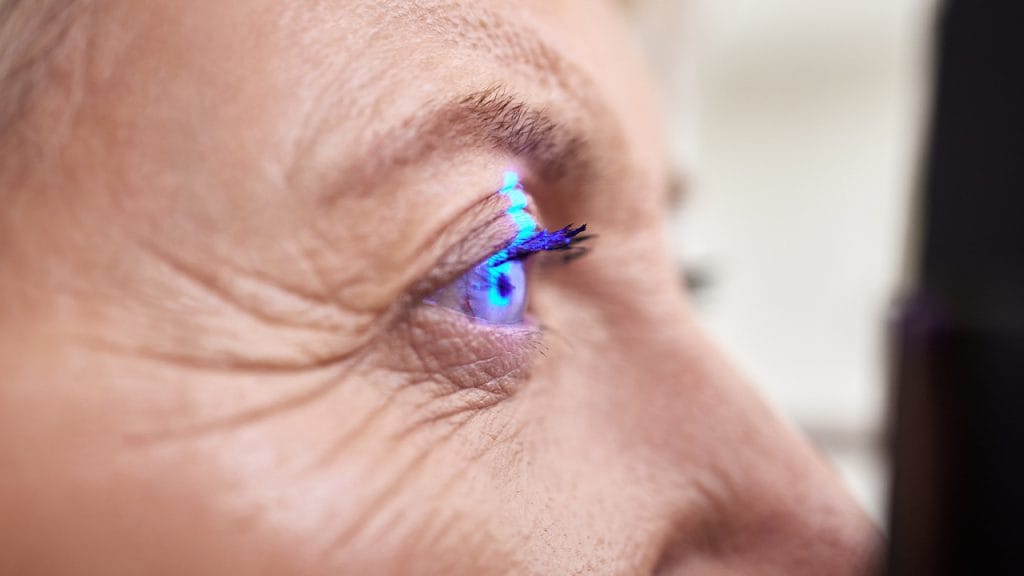
Diabetic retinopathy is a serious eye disease that occurs as a result of damage to the retinal vessels at the back of the eye due to diabetes. The retina is a critical structure where the eye perceives light and performs the visual function.
Diabetic retinopathy damages the retinal vessels when blood sugar levels remain high for a long time; this can result in vision loss and even permanent blindness.
Diabetic retinopathy symptoms are usually not noticed until the disease progresses. However, over time, symptoms such as blurred vision, flashes of light, sudden vision loss and dark spots in the field of vision may occur. Diagnosis is made with eye examination and advanced technological imaging methods such as optical coherence tomography. Diabetic retinopathy treatment includes laser therapy, anti-VEGF injections and surgical methods.
This article covers in detail what diabetic retinopathy is, its causes, symptoms, risk factors and treatment methods. At the same time, suggestions for protecting eye health and frequently asked questions are answered, providing a comprehensive guide for the reader.
What is Diabetic Retinopathy?
Diabetic retinopathy is the most common and serious eye complication of diabetes. The retina is fed by thin blood vessels, and these vessels can be damaged over time due to high blood sugar and form abnormal blood vessels. Since these new blood vessels are weak, they can easily bleed and cause vision problems.
The retina is the most important structure at the back of the eye, and a disorder that develops here directly affects central vision. During a detailed eye examination of the pupil, microvascular changes in the retina can be detected at an early stage. For this reason, it is vital for individuals with diabetes to have an eye examination at least once a year.
Diabetic Retinopathy Symptoms
Diabetic retinopathy symptoms vary depending on the stage of the disease. It may not show symptoms in the early stages, but the following complaints occur in later stages:
Blurred or wavy vision
Floaters in front of the eyes
Light flashes and shadows
Fades in colors
Dark areas in the field of vision
Sudden vision loss
Macular edema can affect central vision and make daily activities such as reading and driving difficult. Retinal thickness and fluid accumulation can be evaluated in detail with optical coherence tomography. When symptoms of diabetic retinopathy are noticed, retinal damage is usually advanced.

Causes of Diabetic Retinopathy
The causes of diabetic retinopathy are directly related to diabetes. High blood sugar levels disrupt the structure of the retinal vessels, forming the main cause of this disease. Over time, these vessels lose their permeability, leak fluid and blood, and can even become blocked, causing new, abnormal vessel formation.
In addition, factors such as long-term high blood pressure, high cholesterol, smoking, and pregnancy also play a role in the development of the disease by damaging the retinal vessels. This pressure on the retinal vessels disrupts the general health of the back of the eye and increases the risk of complications.
Risks of Diabetic Retinopathy
Diabetic retinopathy risks are closely related to the person’s general health status. The highest risk group consists of individuals who have had diabetes for many years and cannot keep their blood sugar under control. The risk is also higher in the following groups:
Those with Type 1 and Type 2 diabetes whose disease duration exceeds 10 years
Those with hypertension and kidney disease
Women who develop diabetes during pregnancy
Those with irregular blood sugar levels
As the risk of diabetic retinopathy increases, new blood vessels form on the surface of the retina. These vessels are weak and fragile. It can cause bleeding, macular edema and serious vision loss. It is recommended that individuals at risk have a retinal examination at least once a year.
Stages of Diabetic Retinopathy
Diabetic retinopathy progresses in four basic stages:
Mild Non-Proliferative Retinopathy: Microvascular changes begin. It usually does not cause symptoms.
Moderate Non-Proliferative Retinopathy: Microaneurysms, small hemorrhages and macular edema may be seen.
Severe Non-Proliferative Retinopathy: The retina goes into oxygen starvation, vascular occlusions become widespread.
Proliferative Retinopathy: New, abnormal blood vessels form. These vessels bleed, causing a risk of sudden vision loss.
Early diagnosis at these stages plays a critical role in protecting the patient’s eye health. If intervention is not made, especially in the proliferative stage, blindness may develop.
Diabetic Retinopathy Diagnosis
Diabetic retinopathy is diagnosed with a retinal eye examination. In individuals with diabetes, the pupil is dilated with drops and the retina is examined in detail. The doctor evaluates bleeding, leakage and abnormal blood vessels in the retinal vessels.
When necessary, the retinal layers are viewed with optical coherence tomography (OCT) and macular edema is detected. In addition, fluorescein angiography is used to evaluate the circulation and vascular structure by administering dye intravenously. Thanks to these methods, early diagnosis can be made and vision loss can be prevented.
Diabetic Retinopathy Treatment
Diabetic retinopathy treatment varies according to the stage of the disease and the level of damage in the eye. The basic treatment options are as follows:
Laser Treatment (Photocoagulation): Destroys abnormal vessels and stops leakage. It is applied with local anesthesia.
Anti-VEGF Injections: Prevents new blood vessel formation. Improves central vision by reducing macular edema.
Corticosteroid Injections: Used to reduce edema.
Vitrectomy Surgery: Applied in advanced cases such as intraocular hemorrhage and retinal detachment.

The most important step in the treatment process is to keep diabetes under control. Blood sugar, cholesterol and blood pressure values should be balanced. In addition, regular eye examinations and optical coherence tomography follow-ups should not be neglected.
How is Diabetic Retinopathy Surgery Performed?
Diabetic retinopathy surgery is a surgical procedure usually performed on advanced stage patients and the most common method is vitrectomy. In this procedure, the vitreous gel that fills the eye is removed; instead, special fluids, gas or silicone oil are placed to support the retina. The surgery is performed under local or general anesthesia and takes approximately 1-2 hours.
The surgeon enters the eye with the help of micro instruments through small incisions opened in the white part of the eye. Bleeding inside the eye is cleaned, abnormal blood vessels and membrane structures are removed. If the retina is detached, it is put back in place.
Laser treatment is applied to the area around the retina to prevent new vessel formation. The gas or silicone oil placed inside the eye helps the retina heal properly.
The patient may be asked to keep his head in a certain position after the surgery. The recovery process can range from a few weeks to a few months. The aim of surgery is to preserve existing vision and stop the progression of the disease rather than regain vision.
Recovery Process After Diabetic Retinopathy Surgery
The recovery process after diabetic retinopathy surgery usually lasts from a few weeks to a few months. In the first days after surgery, stinging, pain, slight bloodshot eyes and blurred vision may be experienced. If gas or silicone oil has been injected into the eye, the patient may need to keep their head in a certain position. This ensures that the retina remains in place and supports healing.
The patient is usually given antibiotic and cortisone eye drops; these drops reduce the risk of infection and control inflammation. The first checks are performed the day after surgery, the first week and the following weeks. During this period, heavy exercise, bending forward and water getting into the eye should be avoided.
Vision improves over time, but this improvement depends on the internal substances (gas, oil) used and the degree of damage to the retina. Although full vision recovery is not always possible, the progression of the disease can be stopped. During the healing process, keeping all systemic values, especially blood sugar, under control directly affects success.
Frequently Asked Questions About Diabetic Retinopathy
1. Does diabetic retinopathy cause blindness?
Yes. Especially in the proliferative phase, permanent blindness may occur when the retinal vessels are seriously damaged.
2. Can diabetic retinopathy be treated?
Yes. With early diagnosis and appropriate treatment, the disease can be controlled and vision can be preserved.
3. How often should eye examinations be performed?
It is recommended that diabetic patients have an eye examination at least once a year.
4. Does vision completely improve after treatment?
It depends on the stage of the disease. Early intervention can significantly improve.
5. Is it possible to protect against diabetic retinopathy?
If blood sugar, blood pressure and cholesterol are controlled, the risk can be significantly reduced.